Meaningful Use Stage 3 to Boost mHealth
CMS's meaningful use stage 3 proposal aims to boost patient engagement through digital tools, requiring providers to leverage mHealth for care coordination.


Popular articles
On March 20th, the Centers for Medicare and Medicaid Services released the proposal for meaningful use stage 3, a 300-page document that the health IT community has been digesting for several weeks. As the comment period ends on May 29th, here is are some key points from the proposed changes and a quick review of their implications for mHealth.Overview Meaningful use stage 3 is the final stage of the Electronic Health Record incentive program that began as part of the HITECH Act in 2009. Meaningful use aims to encourage more eligible providers to use Health IT tools, especially by promoting collaborative and efficient patient care through health information exchange and EHR interoperability.Stage 1 of meaningful use set up requirements for the capture of patient health data by incentivizing EHR use. Stage 2 focused on health information exchange - the exchange of health data between health care providers to improve care coordination. Stage 3 has three broad goals: simplify the program established in stages 1 and 2; advance the use of health IT to improve health care delivery; and align the program with other quality and value programs.The Department of Health and Human Services has proposed a set of 8 objectives that would help achieve the goals of this final stage of meaningful use, which would begin an optional 1-year reporting period in 2017 and become mandatory for all eligible professionals and hospitals in 2018. SearchHealthIT gives a nice overview of the measures and timeline with bullet points for objectives like “electronic prescribing” and “health information exchange.”Legislating mHealth?Most relevant to the mHealth community are the proposed requirements that would advance health IT to improve care - rules that some say are making mHealth tools a necessity. While this may herald the arrival of meaningful use into the 21st century, others worry that legislating mHealth tools will put overworked providers under too much pressure to change their workflows.For example, the proposed rule highlights three specific measures of “patient engagement,” two of which providers would have to meet to qualify for Objective 6: Coordination of Care through Patient Engagement. They are summarized on page 105, or in this analysis by John Halamka CIO of Beth Israel Deaconess Medical Center:
- 25 percent of a provider's patients must access their records through View/Download/Transmit or an ONC-certified app
- 35 percent of patients must receive a clinically relevant secure message
- Providers must incorporate information from patients on "non-clinical" settings from 15 percent of their patients
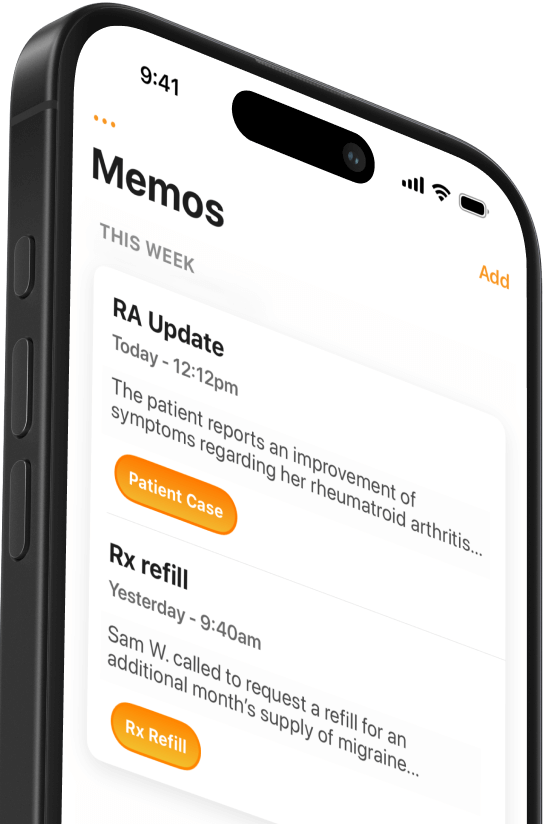
There is some back-and-forth about whether or not providers will be overwhelmed by these criteria if the proposed rule stands. For example, the third measure requires patient-generated data (like physical therapy or health wearable technology) and has some providers worried that they will be assessed on factors outside of their control. However, as Ricky Bloomfield (Duke Medicine’s director of mobile technology strategy) wrote, "It's critically important that we encourage direct engagement and interaction between patients and providers, and this measure intends to do just that.”If the proposed rule stands, mHealth vendors can expect to benefit greatly from the final stage of meaningful use, with additional customers and markets expanding as providers try to interface with patients in new ways or collect data from their health wearables. The recent release of Apple Watch (with its health and fitness functions) is an obvious example, but platforms that facilitate secure messaging (like our own Mobius Mobile app) would also see higher demand.
Related Articles

We Get Doctors Home on Time.
Contact us
We proudly offer enterprise-ready solutions for large clinical practices and hospitals.
Whether you’re looking for a universal dictation platform or want to improve the documentation efficiency of your workforce, we’re here to help.





