How to improve clinical documentation AND doctors' work days
New research confirms physicians spend two hours on EHR work for every one with patients—and documentation burdens continue to rise. What's the solution?


Popular articles
As the healthcare industry leans into value-based care models, providers are more focused on operational efficiency than ever before. In many cases this means more clinical documentation improvement programs, long championed as a way to achieve the Triple Aim of improved outcomes, patient experience and lower costs of care. But what does this mean for physicians?A recent study offers one answer - more time at the desk and less time with patients. Published last year in the Annals of Internal Medicine, the results show that for every hour physicians spend with patients, nearly two hours are spent on EHR and desk work. According to lead author Christine Sinsky, VP of professional satisfaction at the American Medical Association, increasing documentation burdens could also be linked to rising burnout rates.
The 2016 study is especially telling when compared to numbers from just a year earlier. Surveys from 2015 showed that doctors spend one-third to one-half of their time on documentation and follow-up. In just a couple of years paperwork has gone from taking up a large chunk to the majority of a doctor’s time.To make matters more challenging, the solution isn’t less documentation. Clinical documentation is necessary to ensure that providers are fully reimbursed for the services they provide and it’s also linked to better patient outcomes. For example, thorough diagnosis documentation supports an in-depth view of patient history and risk factors, enabling clinicians to better tailor care programs to an individual.
So how can doctor’s improve documentation techniques to make sure they are getting as much info as possible into the patient’s chart - without extra time-consuming work?A familiar solution is documentation support, either with a dictation service or documentation assistant. Medical transcriptionists - whether accompanying the physician or working remotely - commonly work alongside physicians to help them manage the heavy documentation load.
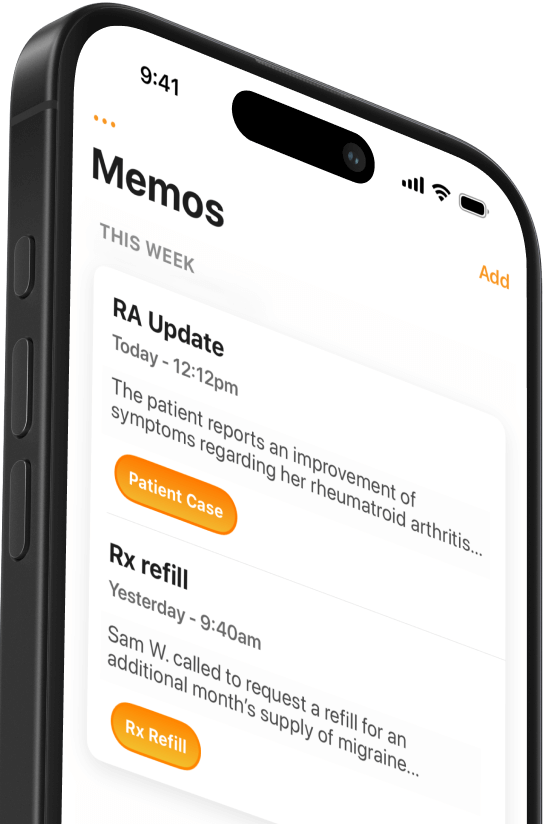
We also know that documentation assistance works. In addition to measuring how doctors spend their day, the 2016 study found that physicians who had documentation support spent more direct clinical face time with patients.As technology improves, providers have started turning to computer-assisted physician documentation (CAPD) strategies to make clinical documentation more efficient and thorough.An example of CAPD is Mobius Clinic, a suite of software applications that make your smartphone an invaluable clinical tool. Mobius Scribe is a Mobius Clinic function that facilitates live dictation at the point of care. Instead of spending hours after the appointment documenting a patient's case and follow-up, Mobius Scribe allows doctors to dictate to a patient’s EHR and instantly have an accurate medical transcription recorded directly in the patient’s record.Mobius Scribe draws on artificial intelligence and natural language processing capabilities developed by Nuance, which also offers a portfolio of CAPD solutions. As Nuance puts it, “Capturing details right at the point of care improves note quality and frees up time for what matters most—patient care.”As doctor’s spend more time documenting and less time with patients, CAPD solutions like Mobius Scribe offer a way forward.
Read about how an orthopedic surgeon is San Antonio uses Mobius Scribe to make his practice more successful, efficient and fulfilling.
Related Articles

We Get Doctors Home on Time.
Contact us
We proudly offer enterprise-ready solutions for large clinical practices and hospitals.
Whether you’re looking for a universal dictation platform or want to improve the documentation efficiency of your workforce, we’re here to help.





