12 key strategies to improve patient communication
Surveys reveal patients want better doctor communication, but busy schedules often make this challenging. Implementing these 12 strategies can improve satisfaction and outcomes.


Popular articles
Surveys have consistently shown that patients want better communication with their doctors. But when physicians face a busy workday, patient communication often gets lost in the shuffle.
As a doctor who interacts with patients every day, you are already a good communicator. But where might there be room for improvement?
Doctors tend to overestimate their communication abilities, so even if you think you’re a great communicator, try to keep an open mind. Continuous learning will improve patient satisfaction, ensure excellent outcomes, and keep you more engaged at work.
Improve patient communication with these 12 strategies
Here are twelve evidence-based strategies to improve patient communication. Pick one you know you could work on and start making it a habit today.
1. Take a seat
The simple act of sitting down can make a conversation feel friendlier and less hurried. Sitting is an excellent strategy because it can improve patient satisfaction without changing the length of your visit.
One study of a neurosurgeon on postoperative rounds found that patients felt the visit lasted longer and rated the visit more positively when the physician sat for rounds (rather than only standing). Create a more welcoming, open atmosphere by sitting for a minute at the beginning of each visit.
2. Greet patients by name
People like to hear their names, and most patients prefer that you address them informally. One recent study found that 99% of hospital patients prefer to be called by their first name or nickname.
Make it a habit to greet patients by name. When in doubt, ask them to clarify their preferred name. This simple question can be a great icebreaker that immediately establishes trust and demonstrates caring.
3. Make eye contact
Studies have found that patients report higher satisfaction when physicians make eye contact during the patient interview. Making eye contact shows patients you are genuinely interested in what they are saying. It conveys empathy, trust, and emotional connection.
4. “BATHE” your patients
The BATHE technique is an evidence-based patient interview strategy that consists of five components. Although it was developed as a form of brief psychotherapy, primary care doctors and other clinicians now use the questions to improve patient communication.
BATHE stands for:
- Background - “What is going on in your life?”
- Affect - “How is it affecting you?”
- Trouble - “What troubles you most about the situation?”
- Handling - “How have you been handling this so far?”
- Empathy - “That sounds very (scary, frustrating, sad, etc.).”
Try using the BATHE questions during inpatient or outpatient care. It will enhance your understanding of a patient’s life experience while improving patient satisfaction and empowerment.
5. Be aware of bias
Another benefit of BATHE interviewing (mentioned above) is that it will help you see patients as individuals rather than as stereotyped members of a group. Everyone has implicit biases, which inevitably affect how you communicate with patients.
Biases are hard to overcome, but acknowledging them is the first step. Then, focus on strategies that help you interact with your patients compassionately. All of the patient communication tips on this list will help you connect with patients as real people, which will minimize the effect of bias in your care delivery.
6. Expect there to be more
When you’re feeling pressed for time, it’s normal to want to move along the visit agenda. One study of family physicians found that when soliciting patient concerns at the outset of a visit, physicians redirected patients’ opening statements after about 23 seconds.
The problem is that patients rarely return to their questions once redirected. A premature interruption can lead to missed information and patients feeling unheard.
Make a habit of always expecting there to be more. Ask: “Is there something else you would like to address today?” Anticipating patients will have more to say than they’ve already voiced will maximize each patient’s chances of receiving the care they seek.
7. Confirm understanding via “teach-back”
Try using " teach-back " to confirm comprehension rather than asking patients if they understood their treatment plan. Simply ask the patient to explain their health issue, intervention plan, or whatever aspect of their care you want to reinforce.
For example, you could say: “Since I’ve prescribed two different medications to you, I just want to confirm you fully understand my instructions, so we don’t miss anything. Please explain to me how and when you will take each medication.”
8. Provide written instructions
As a physician, it can be hard to remember the extent to which your patients are non-experts. Patients are often overwhelmed by a new diagnosis or confused by complex plans for home care or taking medications.
One essential patient communication strategy is to provide written instructions whenever possible. Set up a simple workflow that allows you to share patient education materials as printed handouts or via a patient portal.
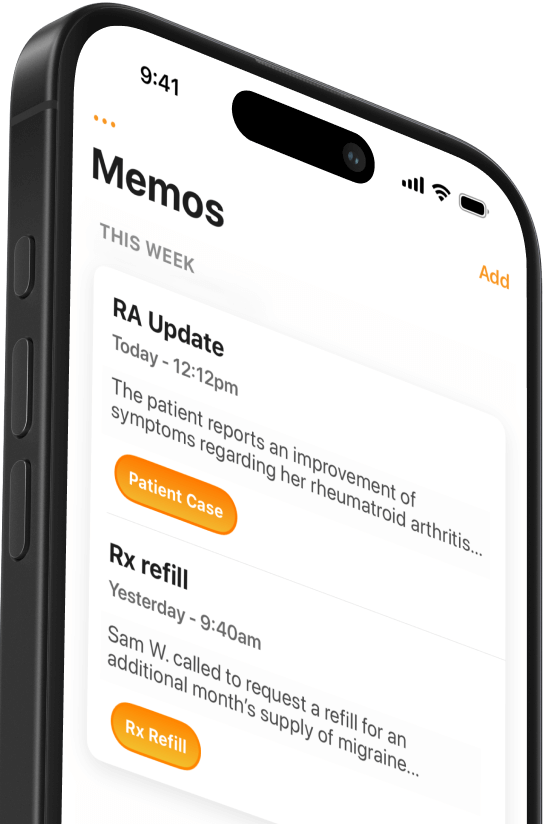
9. Use purpose-build technology
Speaking of patient portals, remember that you have many methods of providing excellent patient communication. In the digital era, telehealth is becoming standard, and patients expect to communicate with their healthcare team through direct messaging.
Use your clinic or hospital’s preferred care management software for secure email or messaging. Maintain timely, efficient communication by setting aside time to respond to your inbox each day.
10. Be reassuring
One of physicians’ most significant challenges is communicating uncertainty. What is the best way to help patients sort through the meaning and implications of uncertainty surrounding their health?
Evidence suggests that patients feel more reassured by having a direct conversation with a physician after receiving diagnostic results. Be reassuring by making a habit of timely follow-up to discuss the next steps with patients after receiving results.
11. Share notes with your patients
The Open Notes philosophy has now become widespread. In April 2021, a new ONC rule mandated that clinicians and hospitals give all patients easy access to their health information, including notes.
Your patients already have access to your notes but consider how this new standard might improve patient communication. Try out these tips for implementing open notes in your practice.
12. Record yourself communicating
When was the last time you watched yourself conduct rounds or see a patient? One of the most potent ways to improve patient communication is to record a video of yourself treating a patient and then watch it.
You will need to find an appropriate setting and get patient consent. You could do this as a mock visit with someone on your staff. Either way, record a video of yourself communicating and review it with a trusted colleague to explore how you might improve.
Take it step-by-step
What do patients want from medical care? They want a relationship with their physician characterized by trust, caring, expertise, and the right amount of autonomy. Promote these elements by focusing on excellent communication in the same way you focus on excellence in medical care.
Try incorporating one of these strategies today until it becomes a habit. By improving your patient communication skills, you can ensure excellent relationships with patients and improve their satisfaction with care.

Related Articles

We Get Doctors Home on Time.
Contact us
We proudly offer enterprise-ready solutions for large clinical practices and hospitals.
Whether you’re looking for a universal dictation platform or want to improve the documentation efficiency of your workforce, we’re here to help.





