What is Team Documentation? Benefits and tips to begin
Team-based documentation reduces physician burden by delegating charting tasks—improving accuracy and patient satisfaction.


Popular articles
As healthcare systems become more complex, physicians are spending more time on administrative tasks, including clinical documentation. Team documentation is a powerful way to streamline patient visits and EHR data entry so the entire team can focus on delivering excellent care.
What is team documentation?
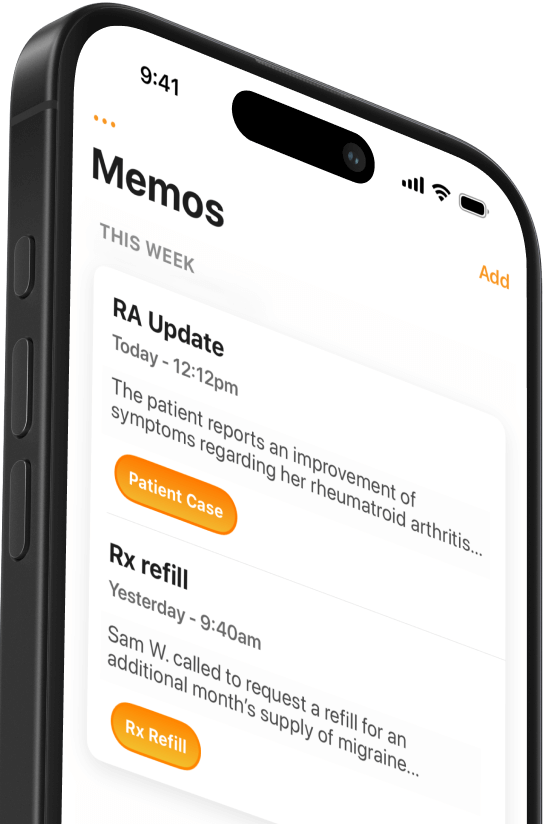
Team documentation is a process where non-physician team members assist with visit notes, entering orders and referrals, reconciling medications, and preparing prescriptions during a patient visit. Non-physician team members can include clinical staff like medical assistants or nurses and non-clinical staff like dedicated scribes.
Consider that most outpatient visits consist of four stages:
- Gathering data
- Physical examination and data synthesis
- Medical decision-making
- Patient education and implementing plan-of-care
In a traditional practice model, the physician is responsible for all or most of these four stages. In contrast, team documentation sets up a workflow that allows medical assistants or other team members to handle much of the data gathering, exam findings, and patient education.
Distributing tasks this way isn’t a new idea. Physicians have discussed team documentation approaches in many articles since around 2010. It is sometimes called “team-based care,” “multiple contributor documentation,” or simply “scribing.”
Examples
Here’s one example of how a primary care visit could play out when conducted using a team-based approach:
- Stage 1: A clinical assistant meets first with the patient to gather data, including chief complaints, often using protocols or a template developed with the physician. The assistant also reviews and makes necessary patient history updates and reviews health maintenance topics, pending orders, and medication lists.
- Stage 2: The assistant presents the case to the physician, who reviews the patient’s chart before entering the exam room with the assistant. The assistant stays for the exam and serves as a scribe, entering a summary of the physician’s findings into the EHR in real time (alternatively, the team uses speech-to-text medical dictation or an AI scribe to capture visit notes).
- Stage 3: The physician formulates a diagnosis and care plan with the patient and clinical assistant. The assistant completes the visit note while the patient has time to ask questions and discuss exam results.
- Stage 4: The physical leaves the room to file orders for the encounter. The clinical assistant remains with the patient to reinforce the physician’s instructions, deliver patient education, and arrange follow-ups.
There are many variations on this example. However, they all follow a well-established plan that results in a well-choreographed “dance” involving multiple care team members.
Benefits of a team-based approach to the EHR
A well-executed team documentation workflow will increase practice efficiency, reduce physicians’ administrative burden, elevate the clinical staff’s role, and improve the patient experience.
Remember that the physician is typically the primary revenue generator in the office. Whenever doctors enter data in the EHR or fill out forms that don’t require their expertise, they’re not spending that time seeing patients and generating income for the practice. By distributing documentation tasks among team members, physicians can focus more on direct patient care, increasing efficiency and productivity.
The American Medical Association (AMA) has a simple tool for quickly calculating how much time and money your practice can save by implementing team documentation.
Of course, team documentation accomplishes more than increased throughput. Here are a few of the other benefits physicians report after implementing team documentation:
- Alleviate burnout: Completing clinical notes before leaving the office improves work-life balance and reduces physician burnout.
- Enhanced accuracy: Collaborative documentation allows for a more comprehensive and accurate representation of patient encounters, reducing the likelihood of errors or omissions in the medical record.
- Standardized documentation: Standardized templates and workflows promote consistency in documentation practices across the healthcare team, ensuring clarity and coherence in medical records.
- Elevate the clinical team: Team documentation can provide valuable professional development opportunities by training nurses, medical assistants, and other staff members to take on new responsibilities and work at the top of their license.
Getting started with team documentation
Setting up any new workflow takes time and upfront effort, especially for physicians. But consider the cost savings and long-term benefits to your well-being.
Here’s some inspiration from a Wisconsin-based family medicine doctor who reported significant benefits from implementing team documentation:
“The only time I’ll ever even look at the computer is if I’m pulling up an X-ray or something. I never document at home. Everything is done and closed by the time I leave the office.”
James Jerzak, MD
So you’re sold on team documentation and ready to try it. Where should you begin?
Fortunately, AMA has a popular Team Documentation Steps Forward module to help you design and improve EHR efficiency with a team-based approach. You’ll create a change team, choose a model, define your workflow, and start with a pilot. Schedule an hour to check it out and get to work implementing a sustainable documentation workflow for your team.
Related Articles

We Get Doctors Home on Time.
Contact us
We proudly offer enterprise-ready solutions for large clinical practices and hospitals.
Whether you’re looking for a universal dictation platform or want to improve the documentation efficiency of your workforce, we’re here to help.





