How to solve the physician shortage
A shortage of 124,000 doctors looms by 2034. Aging patients, retirements, and residency caps fuel the issue—but solutions exist beyond training.


Popular articles
The physician shortage in the United States is significant and growing. Current projections anticipate a national shortage of up to 124,000 physicians by 2034. The shortage includes 48,000 primary care physicians and 77,100 specialists and is especially concerning in rural and underserved areas.
Why is there a shortage of doctors?
Taken as a simple supply and demand problem, a confluence of factors drives the physician shortage:
- Aging Population: The number of people in the U.S. age 65 and older is expected to nearly double by 2060. People typically require more medical care as they age, particularly for chronic conditions like heart disease, diabetes, and arthritis.
- Physician Retirement: The Association of American Medical Colleges (AAMC) estimates that two out of five active physicians will be 65 or older within the next decade. This impending wave of retirements will compound the shortage.
- Residency Bottleneck: Medical schools have increased enrollment to address the shortage, but the number of residency positions hasn’t kept pace. This bottleneck limits the number of new physicians entering the workforce each year.
- Geographic Distribution: Physicians are unevenly distributed across the country, with rural and underserved urban areas facing the most severe shortages. Many physicians prefer to practice in urban and suburban settings with more professional opportunities, better amenities, and higher incomes.
- Physician Burnout: High levels of professional burnout lead to physicians reducing work hours or even retiring early.
Note that the physician shortage doesn’t affect everyone equally. Seventy-five million Americans live in a region designated as a “Health Professional Shortage Area” (HPSA) that lacks access to providers. The map below shows the total population living in HPSAs by state.
Map Showing Total Population Living in Designated Health Professional Shortage Areas

Source: Kaiser Family Foundation and Health Resources and Services Administration (HRSA)
Strategies to address the physician shortage
At first glance, solving the physician shortage seems straightforward: train more doctors. But the situation isn’t that simple.
Every year, over 4,000 Americans graduate as doctors from allopathic, osteopathic, and international medical schools but aren’t matched with a residency training position. Without residency, recently graduated doctors can’t become physicians and serve the public, creating a graduate medical education (GME) bottleneck. One proposed legislative solution is the Resident Physician Shortage Reduction Act, which would direct Medicare money to fund additional residency positions at hospitals in rural areas and HPSAs.
Getting more trained doctors in residency positions is an important initiative. However, others argue that the problem isn't primarily that we have too few doctors. Rather, we’re doing a bad job of using our current physician population efficiently.
New strategies emerge when we examine new care models and approaches that better use existing physician time.
Telehealth is one promising solution, especially for addressing the physician shortage in rural areas. Federal and state policies increasingly support expanding telehealth services, especially since the COVID-19 pandemic.
Interprofessional team coordination is another solution that focuses on more effectively distributing the workload between physicians, nurse practitioners, physician assistants, and other healthcare providers. This approach is particularly beneficial in community-based geriatric healthcare, addressing the specific needs of elderly populations.
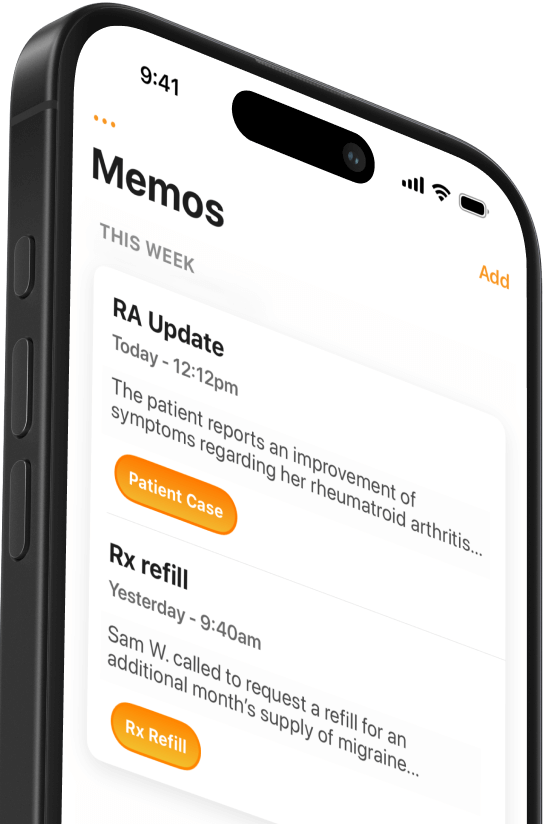
Team Documentation can also streamline patient flows and allow the entire healthcare team to practice closer to the top of their license. Other documentation solutions, like speech-to-text medical dictation or an AI scribe, can free up physicians' time to see more patients.
Increasing the number of patients a doctor sees in a day may seem like a counterintuitive strategy to address shortages in a workforce already plagued by high levels of burnout. However, most doctors say treating patients is the best part of their job. By shifting time from administrative to clinical work, streamlined clinical documentation can help mitigate the physician shortage while healthcare institutions work toward broader structural reforms.
Related Articles

We Get Doctors Home on Time.
Contact us
We proudly offer enterprise-ready solutions for large clinical practices and hospitals.
Whether you’re looking for a universal dictation platform or want to improve the documentation efficiency of your workforce, we’re here to help.