What is the Quadruple Aim of healthcare?
The Quadruple Aim builds on healthcare's Triple Aim by adding provider wellbeing as essential for success. Without thriving care teams, patient outcomes suffer.


Popular articles
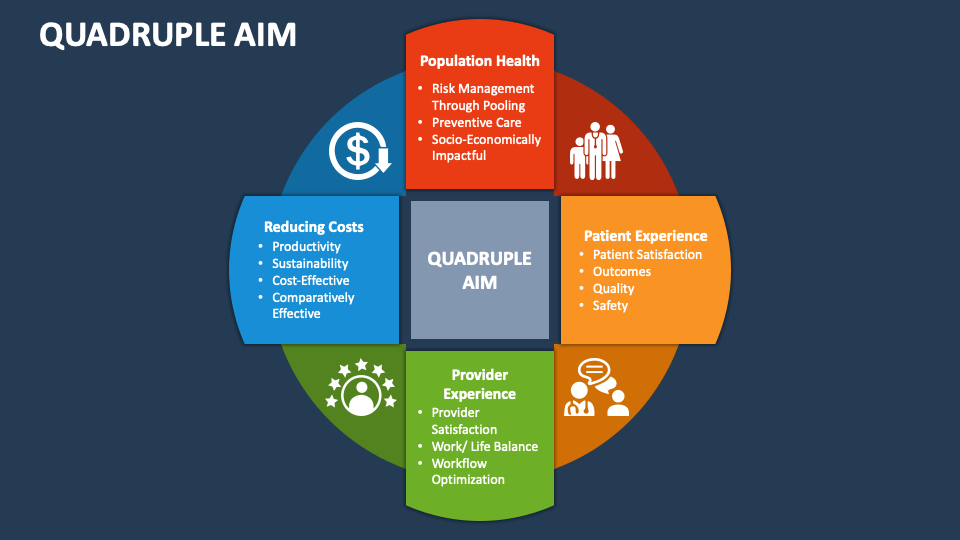
The Triple Aim of healthcare refers to three goals: enhancing the patient experience, improving population health, and reducing costs. However, in the past decade, physicians and healthcare leaders have realized that we can only accomplish the Triple Aim if the care team also thrives at work. As a result, the Quadruple Aim of healthcare is a holistic approach to health systems improvement that focuses on provider wellbeing.
Unpacking the Quadruple Aim
Let’s look more closely at the four elements of the Quadruple Aim of healthcare.
1. Enhancing the patient experience
At its core, the Quadruple Aim is about improving patients' lives. Enhancing the patient experience includes improving healthcare equity, access to care, communication, and patient outcomes and safety.
2. Improving population health
Beyond the traditional emphasis on individual patients, the Triple Aim defined population health as an essential focus.
Organizations have extended their efforts beyond the clinical setting to address social determinants of health such as housing, education, and nutrition. By collaborating with community partners, healthcare institutions can support prevention, early intervention, and long-term health management.
3. Reducing the per capita cost of healthcare
The Triple Aim framework recognized that comprehensive healthcare improvement requires addressing rising healthcare costs. In addition to the other aims, this goal of fiscal responsibility has led to innovative approaches like value-based care models and enhanced care coordination.
4. Enhancing provider wellbeing
The Quadruple Aim builds on the initial three priorities by focusing on caring for those who provide care—the healthcare professionals themselves. This aim is often called “joy in work” or “improved physician experience.”
In 2019, healthcare leaders declared physician burnout a public health crisis, making connections between provider wellbeing, patient safety, and the quality of care. The burnout problem persists; in 2024, about half of doctors said they were burned out.
While burnout awareness has prompted doctors to focus more on their work-life balance, healthcare organizations are addressing administrative burdens and supporting care team mental health.
Who coined the term “Quadruple Aim”?
In a 2014 article, Dr. Thomas Bodenheimer and Dr. Christine Sinsky introduced the idea of a Quadruple Aim in healthcare. The authors proposed expanding the Triple Aim concept, which the Institute for Healthcare Improvement coined and popularized.
In their article, Dr. Bodenheimer and Dr. Sinsky emphasized that physician burnout is associated with lower patient satisfaction, reduced health outcomes, and increased costs. They state clearly: "Burnout among the health care workforce threatens patient-centeredness and the Triple Aim.” In short, there is no Triple Aim without a Quadruple Aim.
How can healthcare systems support provider wellbeing?
There are many strategies for improving healthcare team wellbeing while reducing costs and improving patient outcomes and population health. Popular solutions include improving documentation efficiency (a pain point for physicians) and care team coordination.
In the original Quadruple Aim article, the authors propose several practical steps:
- Implement team documentation so that nurses, medical assistants, and other staff can assist with EHR documentation, order entry, prescription processing, and charge capture.
- Use pre-visit planning and pre-appointment lab testing to reduce time wasted on the review of follow-up results.
- Expand roles to allow nurses and medical assistants to manage preventative care and chronic health coaching under physician-written standing orders.
- Co-locate teams so physicians work in the same space as their team members (research indicates this increases efficiency).
- Ensure that staff who assume new responsibilities receive training and support.
Since Bodenheimer and Sinsky introduced the Quadruple Aim concept in 2014, healthcare technology has improved immensely. EHRs have evolved from novel tools to routine software, and AI is driving a new era of clinical documentation. In addition to better team coordination, tech tools like speech-to-text medical dictation and AI medical scribes can streamline clinical documentation so doctors can spend more time with patients and leave administrative work at the office.
Related Articles


We Get Doctors Home on Time.
Contact us
We proudly offer enterprise-ready solutions for large clinical practices and hospitals.
Whether you’re looking for a universal dictation platform or want to improve the documentation efficiency of your workforce, we’re here to help.