Will ambient clinical intelligence solve healthcare’s documentation problem?
Ambient clinical intelligence captures patient conversations and enters them into EHRs. Can this tech give doctors their time back?


Popular articles
Nobody went to medical school so they could spend hours a day entering data into an EHR. However, surveys show that many doctors spend over 15 hours weekly on paperwork and administration. Could ambient clinical intelligence be the solution?
If you’re thinking, “Ambient clinical… what?” you’re in the right place. In this article, we’ll explain ACI for healthcare providers and discuss why it might improve your workday in the near future.
What is ambient clinical intelligence?
Ambient clinical intelligence (ACI) is an AI-powered voice recognition technology that can capture patient-provider conversations and turn them into accurate clinical notes.
The benefit of ACI is that it operates discreetly in the background, essentially automating the tedious EHR work that currently eats up so many doctors’ workdays. ACI performs this magic using speech recognition technology, natural language processing, and artificial intelligence - all technologies that have improved immensely in the last five years.
“What this means is that the doctor’s notes essentially write themselves, while the doctor is able to give their full attention to the patient and freed from spending two or three hours every evening typing up notes and tackling administrative work.”
- Gregory Moore, MD
Examples of ACI technology
Most providers have heard about AI medical scribes, the primary type of ambient clinical intelligence. The democratization of generative AI in 2023 led to many new players in the space, but a few companies have been working on ACI for nearly a decade.
Augmedix was one of the early companies to use AI for ambient clinical documentation. Their flagship product is a mobile app that uses ambient AI technology and structured data to create fully automated draft medical notes.
Another large player in the ACI space is Nuance, the company behind Dragon Medical Dictation, which was acquired by Microsoft in 2022. Nuance’s ACI technology is DAX Copilot, which is now embedded in Epic EHRs.
Many smaller but growing companies also make ACI solutions. A few popular examples include:
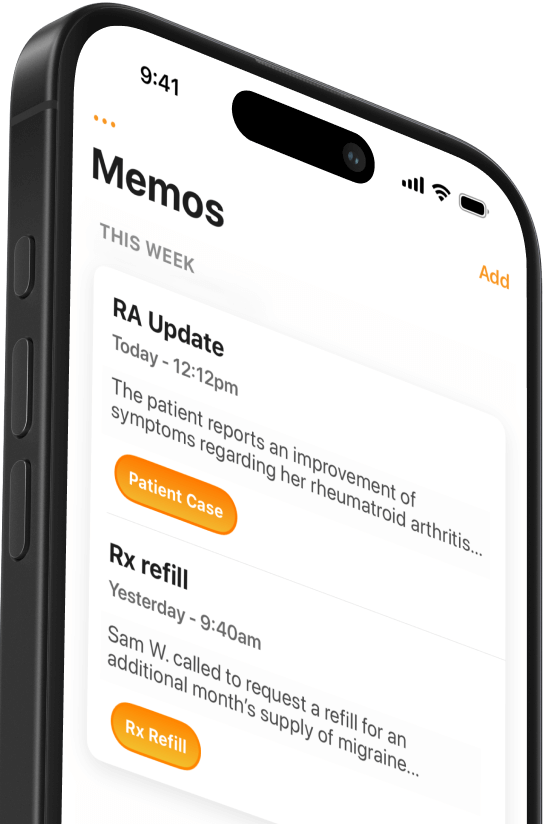
- Conveyor AI: Conveyor AI uses an iPhone app that allows doctors to bring ambient clinical intelligence to any EMR on any Mac or PC. The HIPAA-compliant software writes 80% of your clinical notes simply by listening.
- DeepScribe: DeepScribe’s iOS application records the patient-doctor interaction and automatically produces a SOAP note that humans review for quality assurance.
- Suki: Suki is a voice-enabled digital assistant that allows doctors to speak naturally and streamline administrative tasks, including EMR data entry.
- Freed: Freed automatically transcribes your patient visit and produces a structured clinical note. The software uses machine learning to learn your style, format, and templates and improve over time.
How to choose an ACI tool
Don’t assume that more prominent players like Nuance make superior products. Nowadays, almost any developer can buy a license to use Chat-GPT’s API, meaning the generative AI technology behind most of these software products is equally powerful. Innovative developers are creating better user interfaces, making software more potable (between operating systems and EHRs), and training the AI to format data in structured clinical notes that physicians can customize.
If you’re considering using an AI medical scribe, take advantage of free trial periods to test-run several products and see which best fits your workflow.

How does ambient documentation work?
From a user’s perspective, ambient clinical intelligence is pretty simple: tell the computer to start listening, complete a regular patient visit, and - voilà! - you have a clinical note. Ensure accuracy and save it in the EHR.
While many early adopters have likened AI scribes to magic, there’s a lot of technology at work to make ACI happen. While we’ll lay it out here, bear with us. After all, if you’re going to trust a computer with drafting your clinical notes, you want to understand what it’s doing.
The basic steps that make ACI work
Here are the basic steps ambient clinical intelligence uses to turn a live conversation into a structured clinical note.
- Audio Capture - The first step is for a computer - often a hospital workstation or provider’s smartphone - to capture audio of a clinical encounter. Many AI medical scribes are packaged as smartphone or tablet apps because providers always have these devices nearby.
- Transcription - As the software records the patient and provider speaking, ACI uses advanced speech recognition technology to transcribe the spoken word into text.
- Language Processing - The computer then uses natural language processing (NLP) algorithms to analyze the text and extract relevant information. NLP allows the system to understand the context of the conversation and extract structured data like medical conditions, symptoms, and treatment plans, which eventually become the clinical note. ACI systems go beyond simple text analysis and seek to understand the meaning and intent behind the conversation. Algorithms accomplish this by recognizing relationships between different clinical concepts, identifying modifiers and qualifiers, and interpreting the nuances of language used in a medical context.
- Structuring Data - The ACI system organizes the extracted information into standardized formats, such as SNOMED CT or LOINC codes. It then structures this information according to predefined templates like a SOAP note.
- Adding Context: In some cases, the ACI system might enhance accuracy by integrating additional contextual information like the patient history, previous clinical notes, or relevant medical guidelines.
- Physician Review & Submission: Once the AI system has drafted the note, a human should always review it to confirm accuracy before adding it to the EHR. Typically, physicians will read the note directly after the patient visit to make any edits before saving it to the chart.
Benefits and challenges
Ambient clinical intelligence has two obvious benefits: reducing provider documentation time and improving patient satisfaction.
It’s no secret that providers want to spend less time in the EHR, especially after hours. Early users of ACI tools report that they’re now spending three minutes closing a chart that used to take fifteen minutes.
Patients have also been affected by the computer’s slow creep into the exam room, and ACI could be a welcome change. While patients generally understand and approve of doctors’ using technology during visits, this behavior also impacts communication. Some studies have shown that patients rate providers who don’t use computers as more compassionate and professional than those who do. Ideally, ACI can reduce distractions and allow providers to be more present and engaged with patients.
Saving doctors’ time is just the tip of the iceberg regarding the possibilities created by ACI. Companies are already using ACI technology to spot indicators of depression and social determinants of health during visits. Augmedix has integrated a “bidirectional nudge,” integrating clinical decision suggestions that appear in real-time while the software listens.
While ACI holds immense potential to reduce the healthcare documentation burden, it raises many concerns, especially regarding accuracy and privacy. ACI systems will occasionally transcribe inaccurately or misinterpret clinical information, making it essential that providers review completed notes for accuracy.
The idea of AI technology listening to patient visits has also raised plenty of eyebrows due to potential security breaches and concerns about user acceptance. Technology developers must take HIPAA seriously while helping providers incorporate ACI systems into their existing clinical workflow.
“There’s a lot of appetite for this technology, yet bringing on a brand new vendor and navigating integrations with your existing EHR can cause friction that slows the speed of adoption.”
- Phillip Tornroth, Elation Health
Are doctors using ambient documentation solutions?
While many ACI solutions are already on the market, most providers haven’t tried them. A 2023 survey of primary care physicians found that 33% had tried an AI-powered medical scribe solution but weren’t especially satisfied.
Chief concerns include needing more advanced personalization features and patient education materials and the ability to automate repetitive processes like lab referral orders.
Doctors still want their EHR vendors to guide them toward the best ACI tools that integrate with their system. This attitude may change in 2024 as new companies release EHR-agnostic medical scribes that work on Mac and PC.
While ambient clinical intelligence is still new, one thing is sure: doctors are ready for a new way of documenting that doesn’t involve typing and clicking checkboxes. As physicians increasingly adopt ACI technology, they’re likely to experience a big decrease in those 15 hours of weekly paperwork and a big increase in work satisfaction.
Related Articles

We Get Doctors Home on Time.
Contact us
We proudly offer enterprise-ready solutions for large clinical practices and hospitals.
Whether you’re looking for a universal dictation platform or want to improve the documentation efficiency of your workforce, we’re here to help.