Reduce after-clinic work with these practical tips
Cut after-hours charting with seven tips—set limits, delegate tasks, and use better documentation strategies to protect your time.


Popular articles
Physician burnout has become a significant problem, largely due to a growing administrative burden on medical professionals. Tasks like prior authorizations, quality reporting, messaging patients, and EHR documentation often overflow into after-clinic work.
Most doctors are more intimately aware of how “charting pajama time” or “EHR date nights” impact their personal lives and well-being.
Organizations like the AAFP are advocating for system-level reforms to alleviate administrative complexity. However, individual physicians can simultaneously implement workflow changes to reduce after-clinic work.
Seven tips to reduce after-clinic work
Here are seven practical tips for reducing after-clinic work. Pick one or two strategies that will benefit you, and make time to implement them this week.
1. Have a reason to leave work on time
When you’re motivated to make a change, you can usually find a way to do it. Think about your “why” for reducing after-clinic work.
Do you want to get home earlier to spend time with your children or partner? Are you committed to getting to the gym more often to improve your health and well-being?
Clearly stating your reason for shifting work habits will help you stay focused and motivated. Try writing your “why” somewhere you’ll see it in the mornings before work.
2. Use previsit planning
Pre-visit planning is one of the best ways to streamline patient visits. Order necessary labs or imaging in advance when you schedule a patient for their next visit.
Medical assistants (MAs) can also help prepare visit materials and handle follow-up tasks. You can create standardized prep sheets for common conditions to empower MAs to anticipate and arrange required tasks, facilitating smoother appointments.
3. Coordinate your team more intentionally
There are probably moments in your workday when you wonder, “Why am I doing this task?” Keep a list of these tasks and try to delegate or automate as many as possible.
Thoughtful delegation benefits your entire team. For example, set up protocols for when your MA can take over for you. MAs can give certain vaccines, enter refills in the EHR for many medications, help with documentation, educate patients, and much more.
Delegating gives you and your staff more opportunities to work at the top of your license, providing professional development opportunities and making everyone feel more engaged at work.
Be thoughtful about what you delegate and automate routine tasks whenever possible. For example, patients should be able to easily schedule and re-schedule appointments online or through an app without any involvement from clinic staff. Similarly, pre-prepared patient education materials for common conditions allow your team to send follow-up instructions with one click. Using the right medical practice software tools can improve the patient experience and save you hours every week.
Pro Tip: Schedule regular team meetings to discuss task delegation and workflow optimization. Encourage open communication and feedback from all team members to identify opportunities for streamlining processes and maximizing everyone's efficiency.
4. Revamp documentation practices
Do you still type your clinical notes? Have you tried the latest speech-too-text dictation software? Medical dictation has become incredibly accurate, and speaking your clinical notes is much faster than typing them. Similarly, more doctors are adopting AI medical scribes that listen to your visits and automatically draft a complete clinical note in less than a minute.
While new workflows like dictation and AI scribes require some upfront learning and practice, they can save you hours a week. In the long run, the ROI of a new documentation workflow pays enormous dividends both financially and in terms of physician well-being.
https://youtu.be/ZDXGbbg9yxg
Conveyor AI is one example of a new generation of AI medical scribes that can complete 80% of your EMR notes, simply by listening.
5. Let go of perfect documentation
Any doctor practicing for years will tell you to embrace imperfection and resist the urge to include exhaustive detail in your notes. Instead, focus on essential information and set up your EHR to work for you.
Customized EHR templates and macros can expedite documentation while reducing chart bloat.
6. Complete most documentation in the room
If you don’t complete EHR documentation during the patient visit, you probably know someone who does. Whether you type, dictate, or use an AI medical scribe, there are good reasons to complete notes during patent visits.
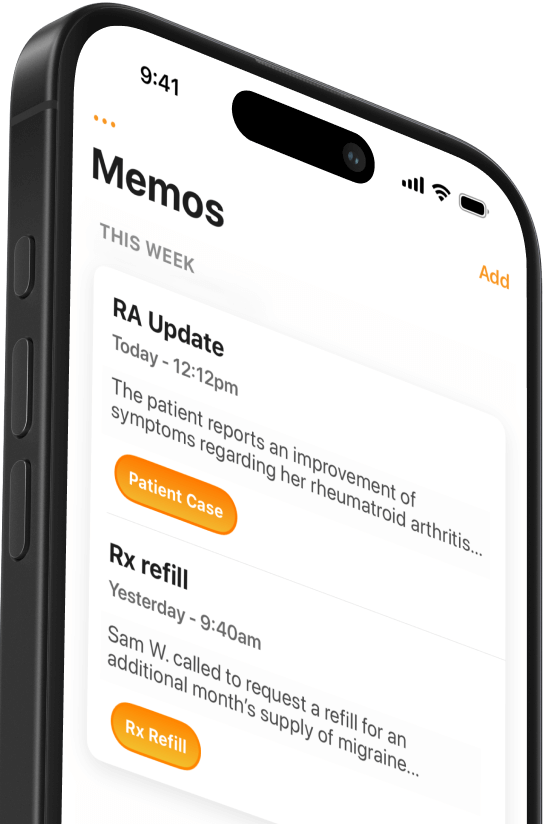
For example, some physicians use a HIPAA-compliant mobile app to dictate notes during patient visits. Rather than end the visit and try to remember everything you covered, dictating during exams ensures accuracy and includes patients in your process. Here’s how one provider explains it:
“I like dictating the history, physical exam, and my plan in front of the patient because I can pause and ask them, ‘Is there anything I should have added or emphasized?’ They like to hear that I can dictate everything, and for me, it’s a matter of convenience that it’s all documented in the moment.”
Dr. Mark Casillas, MD
In addition to dictating in the room, consider a team documentation approach. For example, you can train MAs to begin documentation during the rooming process so the record is started before you start the exam.
7. Implement one-touch messaging
In the patient portal era, efficiently handling incoming messages is essential to prevent inbox overload.
Set up your EHR inbox so messages go to the appropriate person directly. You might also designate a staff member to triage and respond to inquiries so messages don’t pass through multiple people.
A “one-touch messaging” approach also requires reading messages only when you have time to respond. Reserve time specifically for message review and action so you can handle follow-up tasks or delegate them immediately.
Make time to save time
Taking steps to improve your work habits can feel like an extra project on top of an already busy schedule. But remember that a few hours upfront can save you hours every week going forward.
Clarify your “why,” then schedule dedicated time to take actions that will streamline your clinical work and reduce after-clinic work.
Related Articles

We Get Doctors Home on Time.
Contact us
We proudly offer enterprise-ready solutions for large clinical practices and hospitals.
Whether you’re looking for a universal dictation platform or want to improve the documentation efficiency of your workforce, we’re here to help.





