Virtual care expanded quickly as a result of the COVID-19 pandemic, and the general consensus seems to be that there’s no going back. As a recent Hero Digital report summarizes, “The pandemic accelerated the shift to telehealth, patient preferences will sustain it.”
Seema Verma, the CMS administrator, has made similar comments:
“I think the genie’s out of the bottle on this one. I think it’s fair to say that the advent of telehealth has been just completely accelerated, that it’s taken this crisis to push us to a new frontier, but there’s absolutely no going back.”
We all know the pandemic accelerated telehealth by necessity. And there’s a general sense of ushering in an era consumers have been waiting for. But what does that actually look like? What are the numbers related to telehealth adoption that physicians should know?
Telehealth & COVID-19: 5 numbers to know
While telehealth is a term with many meanings, we’re using CCHP’s broad definition: electronic technology used to provide health care and services to a patient when the provider is in a different location.
Statistics like these always have limitations, but they can provide a useful overview of our current moment in virtual visits and healthcare technology.
Hare five numbers to keep in mind when considering the state of telehealth since the COVID-10 pandemic began.
1. Nearly half of Medicare primary care visits were provided virtually in April 2020
Early in the COVID-19 pandemic, HHS temporarily lifted longstanding barriers to expanding virtual care. This new flexibility accelerated clinician and patient use of visits conducted via phone or video.
During April 2020, nearly half (43.5%) of Medicare primary care visits were provided via telehealth. Prior to the pandemic, this number was less than one percent.
This rapid increase in adoption means that healthcare got a chance to test-run telehealth, and overall it performed well. For example, data from Medicare Advantage showed that 91% of seniors on those plans reported a favorable remote care experience.
2. 2 out of 3 people have used telehealth at least once
During the pandemic, the general population seemed to be using telehealth at similar levels to the Medicare population. In 2020, surveys found that 46% of respondents were choosing virtual care to replace canceled in-person healthcare visits.
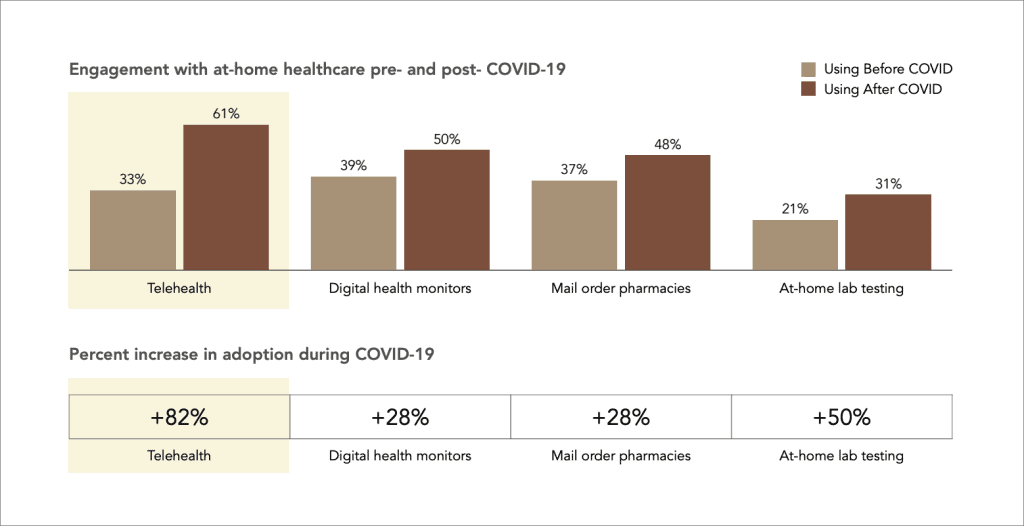
In an August 2020 survey, nearly two-thirds of people said they had used telehealth at least once (61%). That’s up from just one-third before COVID-19.
The same study found that COVID-19 also saw increased adoption of digital health monitors (+28%), mail order pharmacies (+28%), and at-home lab testing (+50%). Taken together, these numbers suggest that most Americans are getting comfortable with remote healthcare.
3. Three-quarters of consumers are interested in virtual care going forward
While the surge in telehealth has been driven by the immediate goal to avoid COVID-19 exposure, the pandemic seems to have changed public perceptions. In 2019, just 11% of respondents to a McKinsey survey said they were likely to use telehealth going forward. By May 2020, that number had jumped to 76%.
According to another survey conducted around the same time, 74% of telehealth users reported high satisfaction with their experience.
4. 7 in 10 providers are motivated to integrate telehealth
Patients’ opinions on the matter seem pretty clear, but what about providers?
One survey of physicians and other clinicians, released in 2021 by the COVID-19 Healthcare Coalition, found that most respondents (78%) said telehealth enabled them to provide quality care during the pandemic. Six in ten thought it improved patient health, and 68% said they were more motivated to integrate virtual care across their practice.
These numbers roughly align with McKinsey data showing that 57% of providers view telehealth more favorably than they did before COVID-19 and 64% are more comfortable using it. While the shift isn’t as dramatic as for healthcare consumers, providers seem slightly more optimistic about this technology as a result of the pandemic.
5. 50 states now reimburse for live video
Policy trends vary state-to-state, with differences in how telehealth is defined, reimbursed and regulated. As of spring 2021, 50 states and D.C.’s Medicaid program reimburse for live video. While all states reimbursed for audio-only care delivery during the pandemic, 15 states are now reimbursing this modality permanently.
You can learn more about federal and state telehealth policies at the National Consortium of Telehealth Resource Centers or the Center for Connected Health Policy.
